Bacterial Vaginosis
ChatRx uses advanced AI to accurately diagnose the symptoms of Bacterial vaginosis and prescribe medications as needed.
Overview
Bacterial vaginosis is a type of vaginal inflammation caused by an overgrowth of bacteria naturally found in the vagina. This condition is the most common vaginal infection in women of reproductive age and can cause unpleasant symptoms, such as a distinctive fishy odor, increased vaginal discharge, and discomfort. While bacterial vaginosis is not considered a sexually transmitted infection, it can increase the risk of other infections and is important to treat promptly.
If you have any signs or symptoms of Bacterial vaginosis, we encourage you to assess your symptoms with our AI-powered online doctor chat.
AI-Powered Symptom Assessment Coming in Spring 2025!
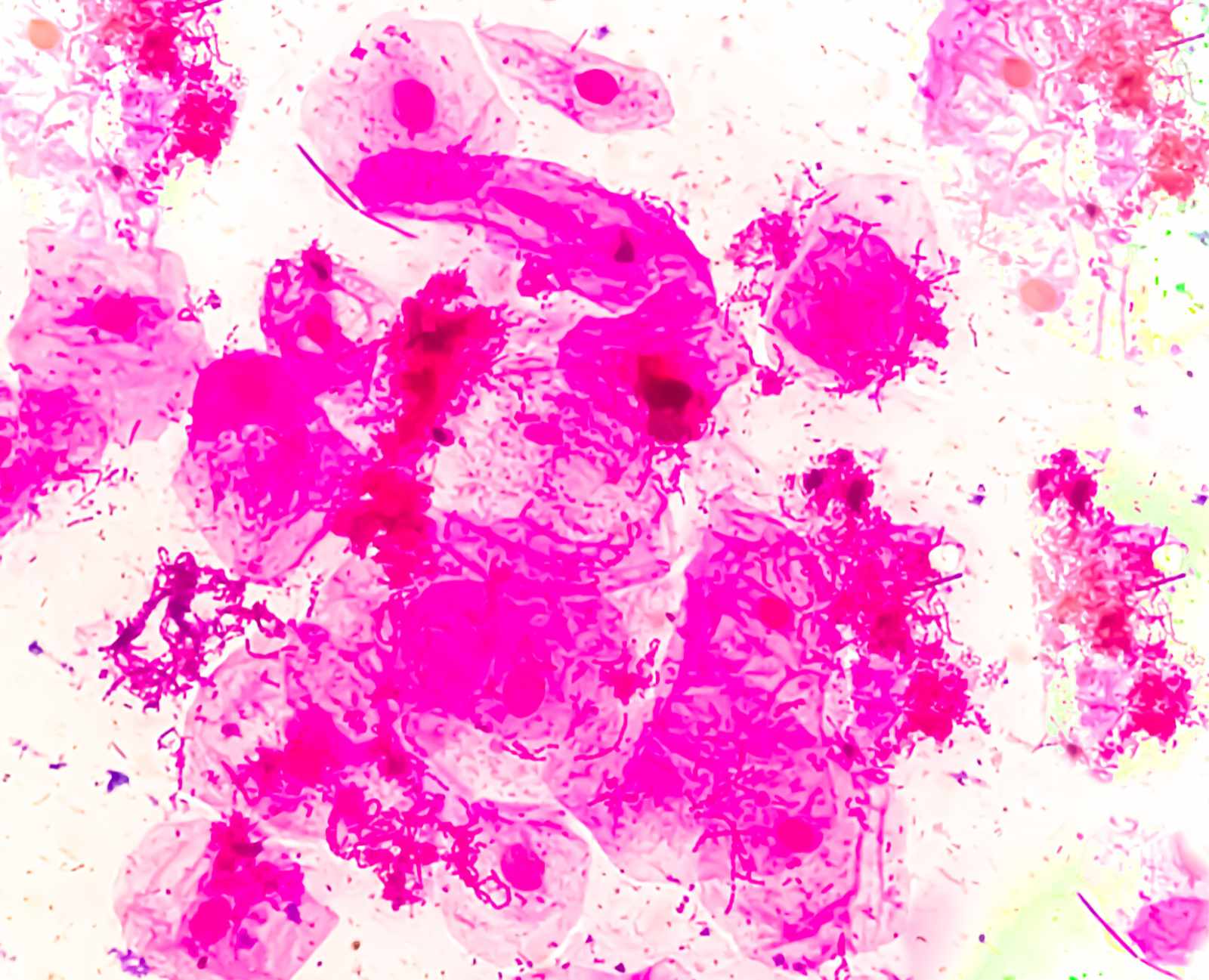
What is Bacterial Vaginosis?
- A type of vaginal inflammation caused by an overgrowth of bacteria naturally found in the vagina
- The most common vaginal infection in women of reproductive age
- Can cause unpleasant symptoms, such as a distinctive fishy odor, increased vaginal discharge, and discomfort
Causes of Bacterial Vaginosis
- An imbalance in the normal bacterial flora of the vagina, often caused by douching or changes in pH levels
- Certain behaviors, such as having multiple sexual partners or using intrauterine devices (IUDs)
- Hormonal changes, such as those experienced during pregnancy or menopause
Preventing Bacterial Vaginosis
- Avoid douching or using scented feminine products, which can disrupt the natural vaginal environment
- Practice good hygiene, including regular bathing and wearing loose, breathable clothing
- Limit the number of sexual partners and use barrier methods, such as condoms, to reduce the risk of infection
Do You Feel Like You Have Bacterial Vaginosis?
AI-Powered Bacterial Vaginosis Treatment Coming This Spring!
Start Your Bacterial Vaginosis Assessment Now
Symptoms of Bacterial Vaginosis
- A distinctive, fishy odor, particularly after sexual activity or during menstruation
- Increased, thin, gray, or watery vaginal discharge
- Burning, itching, or irritation in the vagina or vulva
Treating Bacterial Vaginosis
- Prescription-strength antibiotic medications, such as metronidazole or clindamycin, taken orally or applied topically
- Over-the-counter probiotic supplements or vaginal suppositories to help restore the natural vaginal flora
- Avoiding sexual activity during treatment to prevent the spread of the infection
Self-Care for Bacterial Vaginosis
- Practice good hygiene, including regular bathing and wearing loose, breathable clothing
- Avoid douching or using scented feminine products, which can further disrupt the vaginal environment
- Refrain from sexual activity until the infection has cleared to prevent the spread of the condition
Feeling Unwell?
AI-Powered Symptom Assessment Coming in Spring 2025!
Antibiotics for Bacterial Vaginosis
- Metronidazole or clindamycin, taken orally or applied topically as a prescription-strength medication
- These antibiotics help to restore the natural balance of bacteria in the vagina and clear the infection
Risk Factors for Bacterial Vaginosis
- Douching or use of scented feminine products
- Having multiple sexual partners or using intrauterine devices (IUDs)
- Hormonal changes, such as those experienced during pregnancy or menopause
Summary
Bacterial vaginosis is a common and treatable vaginal infection that can be effectively managed with the right treatment and preventive measures. By understanding the causes, symptoms, and appropriate care for this condition, individuals can take steps to maintain a healthy vaginal environment and prevent the recurrence of bacterial vaginosis.
Frequently Asked Questions
Bacterial vaginosis often causes a thin, gray or watery vaginal discharge with a distinctive fishy odor, especially after sexual activity or during menstruation. It may also cause burning, itching, or irritation. If you’re unsure about your symptoms, ChatRx can help you evaluate them when it becomes available.
It is caused by an imbalance in the natural bacteria in the vagina. Factors like douching, hormonal changes, multiple sexual partners, or using intrauterine devices (IUDs) can disrupt the vaginal environment and lead to bacterial vaginosis.
Although both may cause vaginal discomfort, bacterial vaginosis typically has a thin discharge with a fishy odor, while yeast infections cause thick, white discharge and intense itching. ChatRx will be able to assist in differentiating between these conditions.
Mild cases of bacterial vaginosis may resolve without treatment, but prescription antibiotics are often necessary to prevent complications. ChatRx can guide you on whether treatment might be needed.
Treatment usually lasts 5-7 days with antibiotics like metronidazole or clindamycin. Symptoms may improve within a few days, but completing the full course ensures effective treatment.
Yes, bacterial vaginosis can recur, especially if the factors causing the imbalance in vaginal bacteria are not addressed. Preventive measures, such as avoiding douching and using unscented products, can help reduce the chances of recurrence.
Unlike many infections that appear suddenly, bacterial vaginosis symptoms often develop gradually over several days. You might notice subtle changes after certain activities like sex or during your period. Many women describe a slow shift in their usual discharge or notice a mild odor that becomes more noticeable over time.
Not sure about your symptoms? Get an instant online medical assessment using ChatRx’s AI technology.
Bacterial vaginosis can return after treatment, with about half of women experiencing recurrence within 12 months. While this is common, it doesn’t mean the initial treatment was ineffective. Some women may need additional preventive measures or modified treatment plans to maintain healthy vaginal bacteria levels. If you experience recurring symptoms, it’s important to have them evaluated, as your healthcare provider may recommend different treatment approaches.
While swimming itself isn’t directly responsible for causing BV, spending time in pools and hot tubs can affect your vaginal health. The real issue isn’t the water itself, but staying in wet swimwear too long and exposure to chemicals that can throw off your natural pH balance. The best approach is to change out of wet swimwear as soon as you can and shower afterward.
Skip the waiting room – ChatRx’s AI doctor service can evaluate these symptoms instantly.
This is a common concern for many women. While BV doesn’t typically cause infertility, it can create some challenges if you’re trying to conceive or are already pregnant. During pregnancy, it’s especially important to address BV since it can increase the risk of early labor. If you’re planning to have a baby or are pregnant, keeping an eye on any unusual symptoms is particularly important.
Here’s some good news – male partners can’t develop BV since it’s specifically related to vaginal bacterial balance. However, if you have a female partner, they might be more likely to develop BV. While partners usually don’t need treatment, it’s worth having a conversation about symptoms if they arise.
Your body’s response to stress can actually impact your vaginal health. When you’re stressed, your immune system might not work as effectively as usual, which could make you more susceptible to BV or make it more likely to come back. While you can’t always avoid stress, finding ways to manage it can help support your overall health, including maintaining a healthy vaginal environment.
While there’s no strict “BV diet,” what you eat can make a difference in your recovery. Foods high in sugar might not be your best friend during this time, as they can affect your body’s bacterial balance. On the flip hand, foods rich in probiotics (like yogurt and fermented vegetables) might help support your treatment. Focus on eating a balanced diet that makes you feel good.
During BV treatment, it’s best to stick with pads instead of tampons. This isn’t just about comfort – tampons might interfere with topical medications if you’re using them. Once you’ve completed your treatment and symptoms have cleared, you can return to using tampons as usual.